Best poster prizes at ‘Building networks 2024: engineering in vascular biology’
The EMBO Workshop ‘Building networks 2024: engineering in vascular biology‘ took place earlier this month at EMBL Barcelona, bringing together vascular biologists and bioengineers from across the world to build research synergies to tackle long standing questions in the field of vascular biology.
For the second edition of this meeting, we had 161 people attending on-site and 40 virtual participants. This was the first time remote attendance was made possible at an EMBL Events conference hosted by EMBL Barcelona and we hope to repeat this participation opportunity in the future. There were eleven fellowships provided by the EMBL Corporate Partnership Programme and EMBO and six prizes kindly sponsored by the European Vascular Biology Organisation (EVBO). We held two poster sessions during which the presenters could discuss their research — their work was then voted for by the attendees and speakers. There were five poster prizes awarded during the meeting along with an additional prize for the best short talk. We are pleased to share with you four of the awarded abstracts.
Irradiation triggers molecular and transcriptional shifts in tumor endothelial cells, supporting their activation and enhancing immune response
Presenter: Iva Šantek
Authors: Iva Santek, Tim Bozic, Gregor Sersa, Bostjan Markelc

Abstract:
Abnormal tumor vasculature is marked by inadequate blood flow and oxygen delivery, causing the formation of hypoxic areas, resistant to radiotherapy (RT). Irradiation (IR) affects not only cancer cells but also the tumor microenvironment, including tumor blood vessels. Intriguingly, besides triggering apoptosis of tumor endothelial cells (TECs), IR can also lead to vascular normalization/remodeling or TEC activation, potentially alleviating hypoxia and facilitating immune cell infiltration. However, the role of IR-induced alterations of tumor vasculature and TECs on the tumor response to RT remains poorly understood. Therefore, we aim to clarify how vasculature responds to IR, focusing on its remodeling and TEC activation. First, we irradiated human HUVEC, EA.hy926, and Hulec5a and murine bEnd.3, 2H11, and SVEC4-10 endothelial cells (ECs) with single doses of 0-10 Gy. IR resulted in a dose-dependent manner reduction of EC proliferation and an increase in EC death. Further, RNAseq analysis of HUVECs irradiated with 2 Gy or 5 Gy showed down-regulation of the cell cycle and up-regulation of immune response and EC activation-related pathways. Similar results were obtained in RNAseq analysis of TECs isolated from irradiated MC38 tumors with prominent up-regulation of genes such as Vcam-1, Vwf, Cd47, Il6, etc. This was then validated with immunofluorescence staining of frozen section of MC38 or CT26 colon carcinoma tumors irradiated with either single dose of 15 Gy or fractionated dose of 5 x 5 Gy for endothelial (CD31, EMCN, and ERG), immune infiltration (CD8 and CD4), and transcription (IRF9) markers as well as for proliferation (EdU) and hypoxia (EF5). Additionally, spatial transcriptomic analysis of CT26 tumors irradiated with a fractionated dose of 5 x 5 Gy showed significant differences in gene expression, including less CD31+ and more CD8+ and EC activation marker MECA-79+ positive areas. Lastly, the effect of IR on ECs is now being validated on a vasculature-on-a-chip model, where irradiated samples are being stained with antibodies marking EC activation. In conclusion, we confirmed that IR reduces EC proliferation and survival. Additionally, it alters TEC gene expression and usage of pathways, supporting TEC activation and augmented anti-tumor immune response.
Characterization of the vasculature in human adipose tissue
Presenter: Ditte Marie Storm
Authors: Ditte Marie Storm, Nikos Sidiropoulos, Julius E.R. Grothen, Gijs H. Goossens, Thomas Åskov Pedersen, Joanna Maria Kalucka

Abstract:
In people living with obesity, the adipose tissue (AT) is at the risk of becoming dysfunctional. Dysfunctional AT has been acknowledged as one of the key processes driving the development of obesity comorbidities such as type 2 diabetes and cardiovascular diseases. Dysfunctional AT is characterized by increased inflammation, insulin resistance and metabolic- and vascular dysfunction. The vasculature of AT plays a major role in AT functionality, as it regulates the continuous flux of nutrients and hormones. We aim to characterize the vasculature in human AT at the cellular level, focusing on determinants and signaling pathways related to regulation of AT blood flow (ATBF). To this end, we will isolate vessels from subcutaneous and visceral AT samples, obtained from bariatric surgeries and perform downstream molecular and functional analysis. In addition, we will analyze AT samples from different study groups including individuals with insulin resistance, people with normal glucose tolerance, people who have been assessed for ATBF, and a control lean and obese group. Primary cells isolated from human AT, including endothelial cells, smooth muscle cells, and pericytes, will moreover be functionally characterized in vitro. In addition, key determinants of ATBF will be studied ex vivo, employing whole-mount immunostainings of human AT. In short, our findings should elucidate the molecular mechanisms and cellular crosstalk that governs the ATBF.
Due to the confidentiality of the unpublished data, we cannot share the poster.
ARHGEF18 is a flow-responding exchange factor controlling endothelial tight junctions and vascular leakage
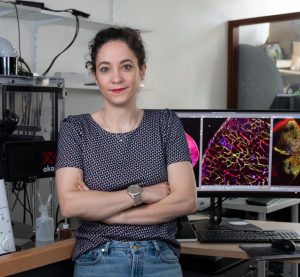
Presenter: Anne-Clémence Vion
Authors: Surya Prakash Rao Batta, Marc Rio, Corentin Lebot, Céline Baron Menguy, Gervaise Loirand, Anne Clémence Vion
Abstract:
The shear stress resulting from blood flow is a major regulator of endothelial cell (EC) biology and morphology. Alteration in shear stress or in its perception results in aberrant EC behavior and has been shown to be associated with vascular disorders. Rho protein mediated cytoskeleton remodeling is an early and essential step of EC responses to flow. However, how Rho protein signaling is controlled by shear stress remains unclear. Combining 3’SRP analysis and Pull Down assays, we identified the Rho nucleotide exchange factor (RhoGEF) ARHGEF18 as a mechanosensitive protein. We demonstrated that it phosphorylation, activity and expression in ECs are modulated by the magnitude of shear stress. We showed that ARHGEF18 interacted with tight junctions, participated in ECs elongation and alignment and allowed the maintenance of the endothelial barrier under physiological flow conditions. ARHGEF18 also promoted EC adhesion and migration by controlling focal adhesion formation. In vivo, using a mice lacking ARHGEF18 in ECs, we observed that ARHGEF18 was involved in flow response of ECs and in the control of vascular permeability during angoigenic processes. Together, our results identified ARHGEF18 as the first flow sensitive RhoGEF in ECs, whose activity is essential for the maintenance of intercellular junctions and the control of vascular permeability in vivo.
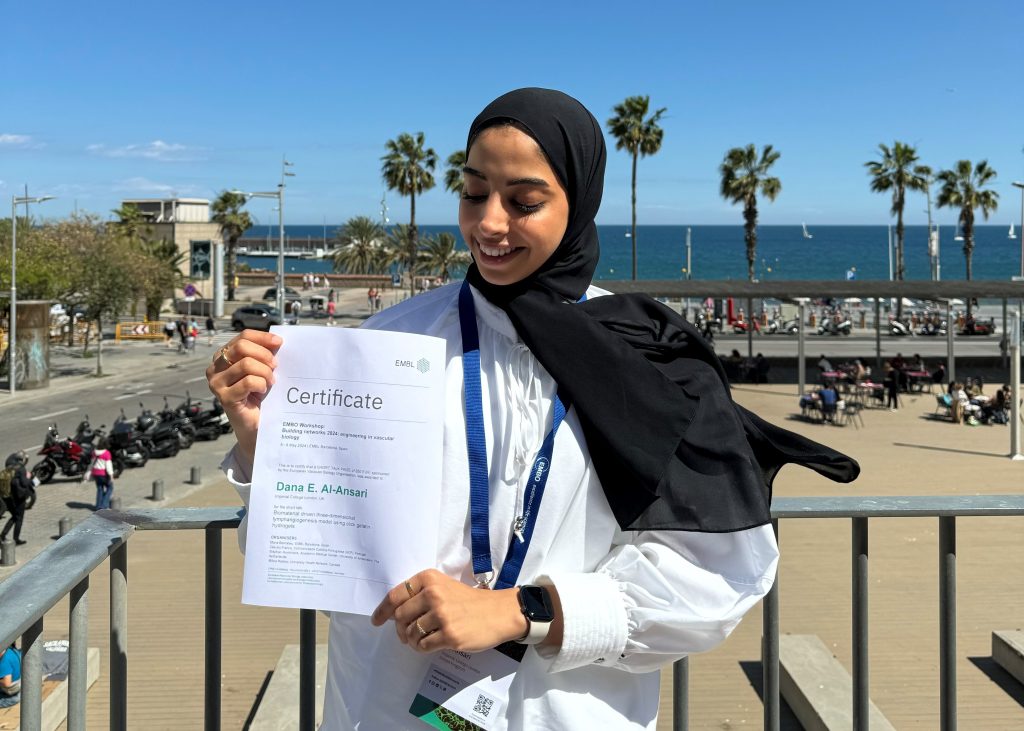
Short talk prize:
Lymphatic endothelial cells mechanoregulation in a three-dimensional tuneable click-gelatin hydrogel model
Presenter: Dana E. Al-Ansari
Authors: Dana E. Al-Ansari, Yangshuo Hu, Cindy Wai, Nicola Contessi Negrini, Daniela Pirri, Adam Celiz, Graeme M. Birdsey

Abstract:
Lymphangiogenesis is the formation of new lymphatic vessels from pre-existing lymphatics. It plays an important role in maintaining tissue homeostasis and immune function. Despite the recent advances in understanding the molecular mechanisms that drive lymphangiogenesis, most studies use conventional 2D monolayer cell culture, which are limited by unconstrained cell migration and x–y plane adhesion. Herein, we established a 3D in vitro spheroid-based lymphangiogenesis model using biorthogonal click-crosslinked gelatin hydrogels (GelTN). The physico-mechanical properties of GelTN were first tailored to closely mirror the endothelium elastic modulus (1.2 – 6 kPa). Using optimised GelTN formulations that supports lymphatic endothelial cells (LEC) encapsulation and viability, we established a LEC spheroid-based lymphangiogenesis assay. Our data showed the robust nature of the 3D lymphangiogenesis model, which was utilised as an in-vitro platform for assays with wide applicability, such as sprouting of endothelial colony forming cells or LEC following siRNA gene inhibition. This has allowed a comprehensive exploration of LEC mechanoregulation in response to matrix stiffness using GelTN. Currently, we are working on a dynamic model of lymphatics, using a handmade uniaxial cell-stretcher device. The cell-stretcher device is made using a 3D printer, programmed using Arduino. The cell-stretcher allowed the exposure of LEC (seeded on GelTN) to mechanical stimulations, that mimic heart contractions (20%, 1Hz). Using this dynamic approach, we aim model cardiac lymphatics and identify mechanosensitive genes of lymphangiogenesis. Overall, the tuneable mechanical properties of gelatin-Tz/Nb provide an avenue not only for tissue engineering but also for clinical applications such as cell therapy or growth factor-incorporated hydrogels for targeted therapy. Our data showed the robust nature of the 3D lymphangiogenesis model, which can be used as an in-vitro platform for assays with wide applicability. This will facilitate the understanding of pro- or anti-lymphangiogenic impact of molecular compounds, genes, and pathways on lymphangiogenesis.

The EMBO Workshop ‘Building networks 2024: engineering in vascular biology’ took place from 6 – 8 May 2024 at EMBL Barcelona and virtually.