New research sheds light on the molecular basis of crib death
Scientists develop a mouse model of Sudden Infant Death Syndrome
Sudden Infant Death Syndrome (SIDS) is a condition that unexpectedly and unexplainably takes the lives of seemingly healthy babies aged between a month and a year. Now researchers of the European Molecular Biology Laboratory in Monterotondo, Italy, have developed a mouse model of the so-called crib or cot death, which remains the leading cause of death during the first year of life in developed countries. The model, published in this week’s issue of Science, reveals that an imbalance of the neuronal signal serotonin in the brainstem is sufficient to cause sudden death in mice.
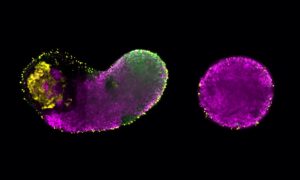
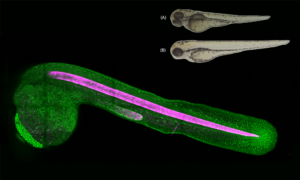
The brainstem, the lower part of the brain that forms the link to the spinal cord, coordinates many fundamental functions including control over cardiovascular and respiratory systems. Victims of SIDS show alterations in those brainstem neurons that communicate using the signalling molecule serotonin. Cornelius Gross and his group at the EMBL Mouse Biology Unit modified the serotonin system of mice to understand the role of this signalling molecule in the brainstem. They overexpressed an important receptor that regulates serotonin signalling, called serotonin 1A autoreceptor.
“At first sight the mice were normal. But then they suffered sporadic and unpredictable drops in heart rate and body temperature. More than half of the mice eventually died of these crises during a restricted period of early life. It was at that point that we thought it might have something to do with SIDS,” says Gross.
Until now it was unclear how changes in serotonin signalling in the brainstem of SIDS infants are involved in sudden death. The findings in the mouse show that deficits in serotonin signalling in the brainstem can be sufficient to cause sudden death and strongly support the idea that a congenital serotonin defect could play a critical role in SIDS.
Serotonin neurons in the brainstem communicate to nerve cells in the spinal cord that innervate the heart and organs involved in temperature regulation such as brown fat tissue. This signalling is defective in the mouse model of SIDS. For example, when placed into a cold chamber the animals cannot properly activate brown fat tissue to produce heat. This inability to activate fundamental body systems under certain conditions is likely to explain why the mice succumb to sudden death.
While a complete block of serotonin signalling does not lead to death, upsetting its intricate balance by overexpressing serotonin 1A autoreceptor can. In response to serotonin the receptor initiates a negative feedback mechanism that reduces serotonin release and dampens down the signal to the body. The researchers caution, however, that it is unlikely that the exact same molecular mechanism leads to SIDS in humans. Nevertheless, the mouse model will help to shed light on how serotonin signalling, when dysfunctional, can be life-threatening.
“We hope the mouse model will help identify risk factors for SIDS. One open question is whether like in SIDS, the animals die during sleep and whether we can identify which mice will die by looking at their heart rate or body temperature before the crisis. Ultimately, we hope it will give new ideas to doctors about how to diagnose babies at risk for SIDS,” says Enrica Audero, who carried out the research in Gross’ lab.