Blocking the waste disposal unit
Detailed structure paves the way for more effective cancer therapies
EMBL scientists and collaborators at the Max Planck Institute for Biophysical Chemistry in Göttingen solve detailed structure of the cell’s waste disposal unit (proteasome) and how it is targeted by cancer drugs. Their surprising results show that cancer drugs interact with the proteasome somewhat differently than previously thought, paving the way for the development of more effective cancer therapies.
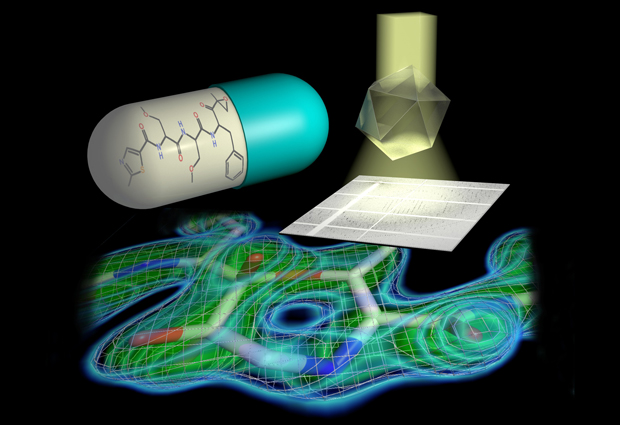
Malignant cancer cells not only grow and divide faster than healthy cells in our bodies, they also produce much more waste. This makes cancer cells more dependent on the cell’s most important waste disposal units, large protein complexes known as proteasomes, which break-down defective proteins and remove them from circulation. Due to this dependence, treatments for some cancers, such as a type of bone marrow cancer known as multiple myeloma, are designed to specifically target the proteasome. Once the activity of the proteasome is blocked, the cancer cell becomes overwhelmed by the build-up in waste, and eventually dies. However, exactly how this mechanism works is not fully understood. Now, a team of researchers from EMBL in Hamburg and the Max Planck Institute for Biophysical Chemistry in Göttingen, have succeeded in solving the 3D atomic structure of the proteasome in unprecedented detail. The results, published in Science, reveal just how cancer drugs block the activity of the proteasome, and pave the way for the development of more effective proteasome inhibitors for cancer therapy.
In order to study the 3D atomic structure of the proteasome, the scientists first had to produce protein crystals of the large protein complex. But such large molecules are notoriously difficult to crystallise. So first an optimised production pipeline was established which enabled the scientists to produce large amounts of protein and crystals before moving for analysis to the EMBL crystallography beamlines on the DESY campus in Hamburg. At the beamline, powerful X-rays are shone at the crystals, creating distinctive patterns as the X-rays bounce off the atoms in the molecule, determining their exact position. As a result of the careful preparation, cutting-edge equipment available to the scientists at the beamline, and the high quality X-ray light source, the scientists were able to reveal a structure of unprecedented detail, down to the position of single atoms. In addition to solving the structure of the proteasome by itself, the group were also able to resolve the structure of the molecule bound together with four different inhibitor drugs, either already in use in the clinic, or currently in clinical trials.
“The substantial improvement in resolution compared to previous research has allowed us to establish the exact chemical mechanism by which inhibitors block the proteasome. This knowledge makes it possible to optimise inhibitor design and efficacy – since only inhibitors tailored to the proteasome shut it down completely,” says Ashwin Chari, project group leader from the Department of Structural Dynamics headed by Holger Stark at the Max Planck Institute for Biophysical Chemistry.
Importantly, their findings revealed a surprising detail in the way the inhibitor drugs bind to the proteasome, and it’s not as scientists previously thought. The results show that in contrast to previous assumptions, a 7-ring structure including a methylene group form at the interface where the proteasome and inhibitor bind. “Even though a methylene group just comprises one carbon atom and its two associated protons amidst the more than 50,000 atoms of the proteasome, it decisively influences which chemical features make the inhibitor most effective in blocking the proteasome,” says Thomas Schneider, who leads the group at EMBL. “This has to be taken into account when developing new inhibitors and searching for new drug candidates,” adds Holger Stark. The researchers have already filed a patent application for the chemical procedure to design such inhibitors. “Clinical applications are always preceded by knowledge about targets – therefore, the details, where every atom counts, make all the difference,” EMBL beamline scientist Gleb Bourenkov concludes.