EMBL-EBI Press Office
Wellcome Genome Campus Hinxton, Cambridgeshire CB10 1SD, UK
media@ebi.ac.uk+44 1223 494369
Researchers find evidence that B cells may be more important in immunotherapy than previously thought
Researchers at EMBL’s European Bioinformatics Institute (EMBL-EBI) and the Medical University of Vienna have found evidence that B cells might play an important role in immunotherapy for melanoma. Currently, immunotherapy is primarily focused on T cells, but the results suggest that B cells could also provide an interesting research avenue.
Immunotherapy is a form of cancer treatment that uses the body’s own immune system to recognise and fight the disease. It comes in a variety of forms, including cancer vaccines, targeted antibodies or tumour-infecting viruses. Only some cancer patients currently benefit from this kind of therapy.
In the case of melanoma, which is a particularly aggressive form of skin cancer, established immunotherapies focus on T cells. T cells play an important role in controlling and shaping the immune system and they are able to directly kill cancer cells, while also recruiting other cells into the process.
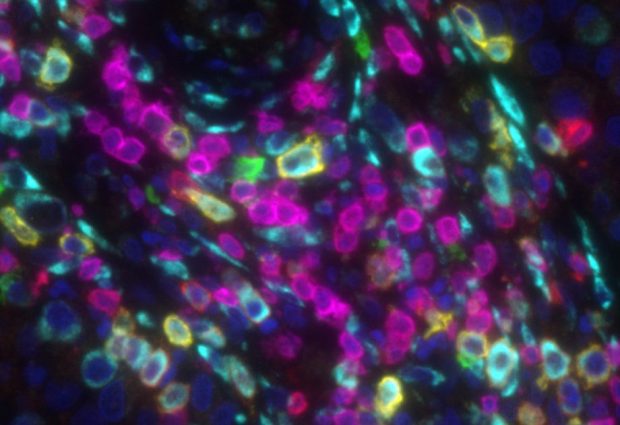
A recent study published in Nature Communications has shown that, alongside T cells, B cells play a critical role in triggering melanoma-associated inflammation. B cells are a type of white blood cell, which can produce antibodies along with several important messenger molecules. The researchers found that, in the case of melanoma, B cells act almost like a satnav, directing T cells to the tumour via the secretion of such distinct messenger molecules.
“Immunotherapy has transformed cancer treatment,” explains Johannes Griss, Researcher at the Medical University of Vienna and EMBL-EBI. “It unleashes T cells so they can fight cancer in a more effective way. For the first time, we found that B cells also play an important part in the process and help T cells find the tumour. The role of B cells in immunotherapy is still largely unknown, but it seems they may have more impact than previously thought.”
During the study, the researchers observed that when B cells were depleted from melanoma patients, the number of T cells and other immune cells dramatically decreased within the tumours as well. In subsequent experiments, the researchers showed that a special subtype of B cells seems to be responsible for guiding T cells and other immune cells to the tumour.
Interestingly, melanoma cells seem to force B cells to develop into this distinct B cell subtype. Most excitingly, this specific B cell subtype also increased the activating effect of current immune therapies on T cells, and higher numbers of this B cell subtype in tumours before therapy predicted that a patient would respond better to subsequent immunotherapy.
“Further research is required to answer questions such as how melanoma cells modify B cells, what mechanism B cells use to support the activation of T cells, and how we can help these B cells to support current immunotherapies in cancer patients,” concludes Griss.
This post was originally published on EMBL-EBI News.