EMBL scientists investigate rare lung disease
Researchers at EMBL investigate the epigenetic changes in a rare lung disease, pulmonary arterial hypertension.

Researchers in EMBL’s Zaugg group have studied the causes of pulmonary arterial hypertension (PAH), a rare disease that causes high blood pressure in the arteries of the lungs. The study, carried out in collaboration with Stanford University School of Medicine, compared lung cells of patients with the disease with those of healthy individuals. Instead of finding a single clear cause, their results showed large epigenetic disturbances – changes that don’t occur in the DNA sequence itself, but are responsible for enhancing or reducing the activity of certain genes. These epigenetic changes can affect the activity of proteins called transcription factors and DNA sequences called enhancers, known as the gene regulatory network. The abnormal behaviour of the lung cells in patients with PAH seems to be caused by a general rewiring of this regulatory network. The results of the study are published in Nature Communications.
Looking for signals
PAH is caused by obstruction of the lung arteries, as a result of proliferation of smooth muscle cells that surround them. This results in high blood pressure and leads to severe health problems. The heart is forced to work much harder to pump blood through the lungs and ultimately weakens or even fails if the disease is not treated by a lung transplant.
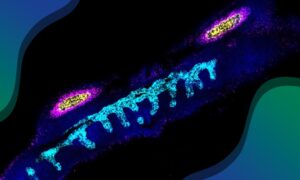
“Most PAH cases aren’t caused by any known mutation,” says EMBL group leader Judith Zaugg, “and there was a hypothesis that the disease is caused by epigenetic changes.” An important class of epigenetic changes are modifications to the DNA–protein complex, known as chromatin. The researchers profiled such chromatin modifications in the cells lining the blood vessels in the lungs of PAH patients, and compared them with those of healthy individuals. They found very large differences in regulatory elements, which are part of the non-coding regions of the genome. These are sequences of DNA that don’t carry instructions for making proteins, but are responsible for other functions such as gene regulation. What the researchers found in the patients’ lung cells was a huge epigenetic rearrangement.
To understand the role of these changes in the disease, the Zaugg group developed a computational tool to reconstruct an enhancer-based gene regulatory network in a specific cell type, which they applied to their data. The results suggested that the rewiring of the regulatory network in the cells surrounding the blood vessels, called endothelial cells, makes it possible for them to differentiate to become smooth muscle cells, which then contribute to the obstruction of the lung arteries.
Observing chromatin states
“The surprising thing was that we were expecting strong differences in the gene expression levels, but couldn’t find anything. Usually, in these types of disease studies, the differences in gene expression are huge,” says Armando Reyes Palomares, a postdoc in the Zaugg group at the time of the study; now at the Complutense University of Madrid. The signal that the researchers were looking for turned out to be entirely in the chromatin states. These states describe modifications of the DNA-protein complex.
One motivation of the study was to understand the disease mechanism of PAH and potentially identify a gene that could be targeted to develop a therapy. “The results are disappointing as far as finding potential drug targets is concerned,” says Judith. “It seems that, in PAH patients, the cell is in a completely different state. It’s not just one single switch that you can turn back.” The results highlight the importance of considering chromatin states during early drug development. “It shows that there is much more information to be found in the chromatin states of a cell, rather than only looking at gene expression levels,” says Judith.
Although no clear drug target could be identified, the researchers gained valuable insights into the mechanisms of the disease. This information will be important for any future drug development efforts. By showing that epigenetic changes may prime endothelial cells to differentiate into smooth muscle cells, which would then obstruct arteries, it also raises the question of what exactly triggers this huge rearrangement. In addition to the insights gained into this specific disease, the study also describes a computational tool to generate gene regulatory networks. This tool can help scientists to understand the impact of epigenetic changes in non-coding regions of the genome. The software is currently used in the Zaugg group to investigate the effect of epigenetic remodelling in several other diseases.
The Stanford | EMBL Life Science Alliance is a non-profit cross-institutional research initiative dedicated to the advancement of science and technology development. Inaugurated in 2015, the Alliance promotes collaboration and exchange, and facilitates access to research services offered at EMBL and Stanford Medicine.