Limiting the damage in stroke




Scientists at the Universities of Heidelberg and Ulm and a unit of the European Molecular Biology Laboratory (EMBL) in Monterotondo, Italy, have discovered that a specific signal within brain cells may determine whether they live or die after a stroke. Their study, published online (November 13) by Nature Medicine,strongly suggests that new therapies for victims of strokes could be developed by controlling a molecule involved in passing the signal.
Strokes lead to death or permanent disabilities for millions of people every year when an interruption of the flow of blood to brain cells deprives them of vital oxygen and nutrients. But the fate of the cells seems to depend on what happens next. Scientists discovered that damaged and dying brain cells are very actively using an internal ‘communications network’ known as the NF-κeB signalling pathway. Cells have many such networks; their function is usually to switch genes on or off, changing the chemistry and behavior of the cell. Most drugs work by interfering with molecules that play important roles within these networks.
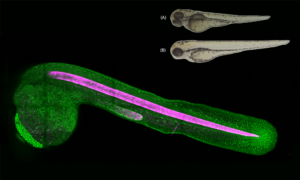
Scientists knew that NF-κeB signaling was active in neurons, but its function was unclear. “We had some evidence that in nerve cells, it could trigger a self-destruction program called apoptosis,” says Markus Schwaninger of the University of Heidelberg, one of the heads of the project. “If that was the case, the signal could certainly be playing a role in the death of neurons after stroke and other types of brain damage.” To address this hypothesis, Schwaninger’s group had established a sophisticated method of creating a stroke-like condition in mice, a model that can be used to investigate new therapies.
What would happen if the activity of NF-κB in neurons were blocked after a stroke? To test this, genetic mouse models were required. The group of Manolis Pasparakis at EMBL’s Mouse Biology Unit developed a strain of ‘conditional knockout’ mouse in which a protein called IKK2, which activates NF-κeB, can be controlled. The researchers are able to shut down the molecule at any time in neurons. “More common methods of shutting down a gene remove it from all tissues, for an animal’s entire life,” Pasparakis says. “You can’t do that with NF-κB itself – in other types of cells the signal has important functions which are necessary for the animal to survive. So to test our hypotheses about its role in neurons, we needed more precise control of the gene.” In parallel, Bernd Baumann and Thomas Wirth at the University of Ulm had generated two additional mouse models, which allow the reversible repression or activation of IKK2 at any time in neurons. “The unique advantage of this system is that we can specifically induce or block this signaling pathway at virtually any time and selectively in neurons,” Wirth emphasizes. Putting all of this expertise together permitted the researchers to get a clear picture of IKK2’s role after a stroke.
Mice with the hyperactive form of IKK2 in neurons and too much NF-κeB signalling, they discovered, suffer even more damage than normal; far more cells die. But if the IKK2 signal is blocked, damaged cells stay alive and even seem to recover. The effects are long-term; neurons in the damaged tissues were still alive several days after the stroke.
Two factors make the study promising in the search for treatments for this deadly disease. First, shutting down the IKK2 signal had beneficial effects even when it was done a few hours after the stroke. That is important when thinking about possible human therapies; it usually takes time for a patient to reach the hospital. Secondly, the same effects could be achieved by blocking IKK2 activity with a small artificial molecule. That’s what a drug will have to do. Human cells have a very similar NF-κeB signaling network, which means that there is a good chance IKK2 will do something similar in our own brain cells. As NF-κeB passes a variety of other important signals, pharmaceutical companies have already been developing molecules that target parts of the signaling pathway.
Press Releases University of Heidelberg